"Artificial Insemination"
Couples who have been trying to conceive for a long time, but have so far failed to achieve a pregnancy often seek medical help and may opt for "artificial insemination", i.e. the use of medically assisted reproduction techniques to fertilize the egg with the male partner's sperm. For this purpose, there are different methods and techniques which are applied depending on the couple's initial situation.
1. Intra-Uterine Insemination
2. In Vitro Fertilization - IVF
3. ICSI
4. IMSI
5. Special Techniques
1. Intra-Uterine Insemination
Intra-uterine insemination can be offered to young women (up to age 36) as a first therapy option for 3 to 6 treatment cycles. What is indispensable here are open fallopian tubes in the woman and normal sperm count and quality (semen analysis) in the man. If those prerequisites are met, a polycystic ovary syndrome in the woman is often the root cause of the undesired childlessness. In this case, follicle-stimulating hormones/gonadotropins or clomiphene are used to induce the maturation of 1 to 2 ovarian follicles. Subsequently, ovulation is triggered by hCG and the processed sperm sample is placed inside the uterine cavity. The spermatozoa travel through the fallopian tubes to meet the egg cell. The fertilization of the ovum by a single sperm cell usually occurs in the ampulla part of the fallopian tube. Then the fertilized egg (zygote), i.e. the resulting embryo starts its 5-day migration along the fallopian tube to the womb. As a blastocyst it reaches the uterine cavity and starts implanting into the uterine lining (endometrium). To ensure that the uterine lining is well-prepared for (nidation/implantation), specific hormones (such as progesterone) have to be administered up to the moment when embryonic heartbeat can be detected via ultrasound about 4 weeks after ovulation. In some cases, progesterone supplementation is required up to the 12th week of pregnancy.
2. In Vitro Fertilization - IVF
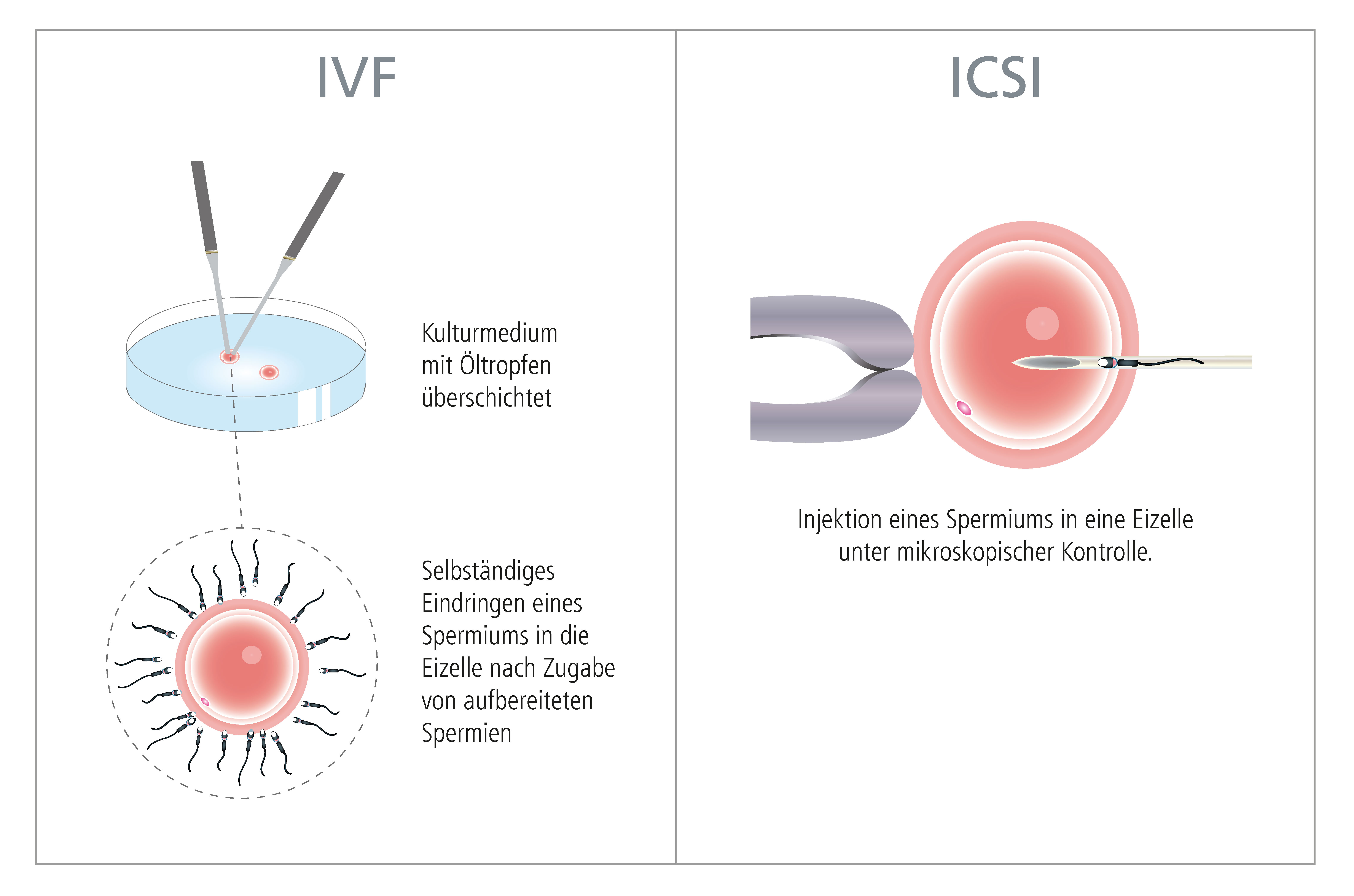
Since 1978, there has also been the possibility of performing in vitro fertilization and subsequent embryo transfer, thus providing a therapeutic option to couples facing tubal factor infertility, various endocrine disorders, azoospermia or poor sperm quality. This approach may be used to realize these couples' dream of having a baby. "In Vitro Fertilization" or "extracorporeal fertilization" is generally understood as the fusion of egg and sperm outside the female body. For this purpose, an oocyte that has been removed from the ovary is combined with the man's spermatozoa in a petri dish (= in vitro). The fertilized oocyte is transferred into a special culture medium and placed in an incubator in order to grow into an embryo (see "Blastocyst Culture"). Cutting-edge laboratory techniques enable the close monitoring and detailed assessment of embryonic development. Once the embryo have reached a certain stage of development (blastocyst = embryo capable of initiating implantation), those with the highest implantation potential (maximum of 2 embryos) are selected an can then be placed into the woman's uterine cavity (see "Embryo Transfer"). This kind of treatment can be extremely challenging for the couple in question. For this reason, the therapy should be customized to take account of the couple's individual needs and should take place in a familiar and friendly atmosphere. The couple needs to be well informed on all aspects of the therapy options available to them. Having reviewed any existing medical results, and after a thorough gynecological examination, analysis of the semen and evaluation of existing diagnostic findings (and medical results yet to be established), an individual therapeutic plan is drawn up. In some cases, it may be useful to consider psychological counseling (see "Emotional Support") ahead of IVF treatment. After a first initial consultation, each couple is provided with a precise description of the individual examinations (follow-up ultrasound examinations, hormone analyses, blood sampling etc.) and details on the medication in the form of a leaflet and a therapy plan. Our treatments are always tailored to the patients' individual needs.
3. ICSI
From 1992, the so-called "Intracytoplasmic Sperm Injection" (ICSI procedure) has become a milestone in the treatment of infertility. The procedure involves injecting a single sperm directly into an oocyte to achieve successful fertilization. The ICSI procedure can be used to help couples in situations where the spermiogram results indicate limited male fertility, e.g. the ejaculated semen does not contain any motile spermatozoa. If, due to ejaculatory duct obstruction, no sperm can be found in the ejaculated semen specimen, sperm can be retrieved from the epididymis. The thus obtained sperm can then be used for ICSI. There is also the possibility of extracting spermatozoa directly from the testis (TESE/TESA).
│ © 2022 Next Fertility IVF Prof. Zech • Member of Next Clinics
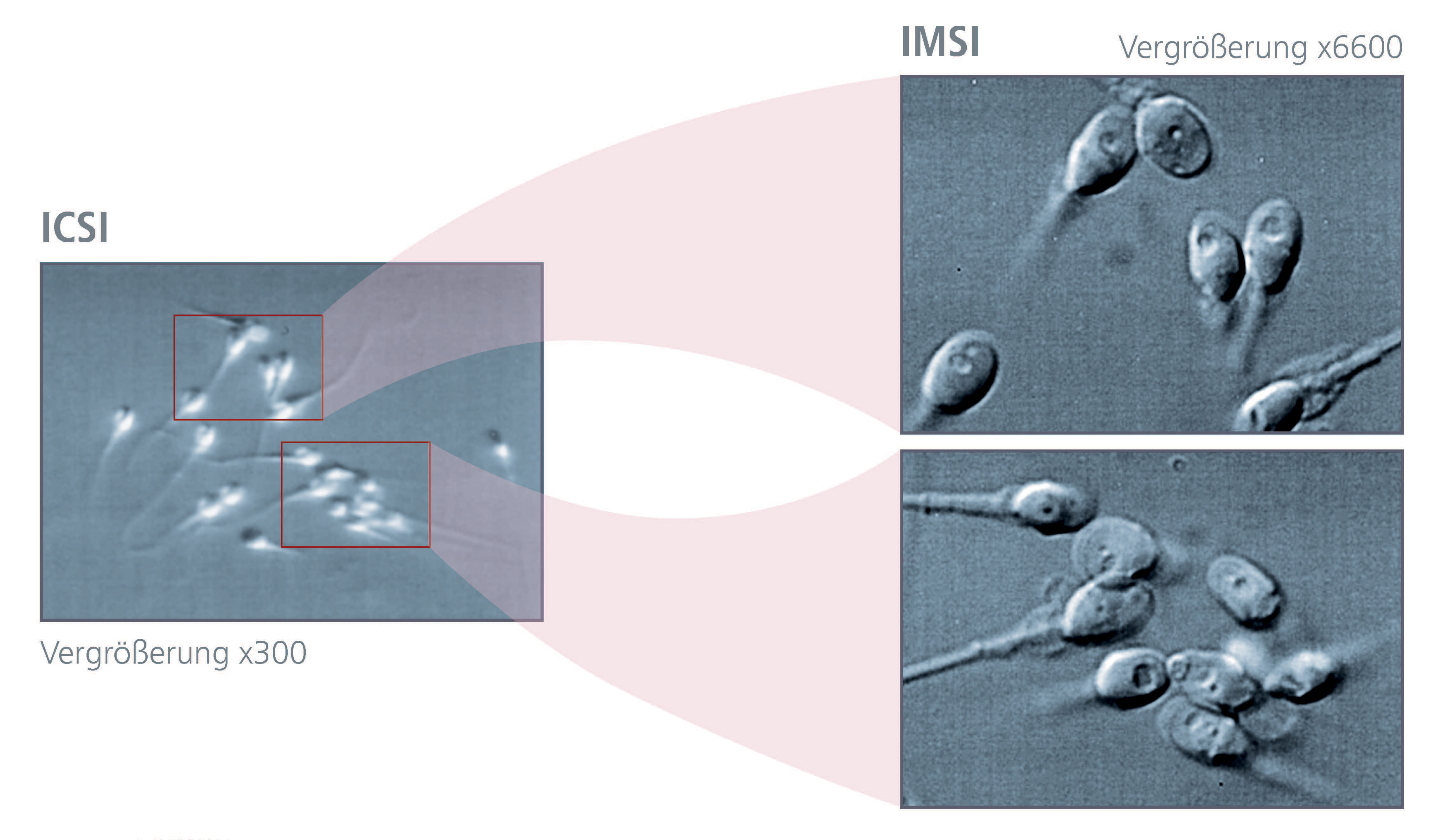
4. IMSI
In "natural" reproduction as well as in conventional IVF (in vitro fertilization) the zona pellucida and the cumulus cells surrounding the oocyte act as a biological barrier that prevents abnormal spermatozoa from attaching to the egg cell, so that in most cases only "normal" sperm are able to fertilize an egg. During the aforementioned ICSI procedure, morphological assessment and selection of the spermatozoa are performed (usually at a magnification of 200-400x) by specialized biologists. The quality of the assessment and subsequent selection can be further enhanced by using high-resolution microscopy for detailed analyses, i.e. "Intracytoplasmic Morphologically Selected Sperm Injection" (IMSI). (See "Sperm Selection").
5. Special Techniques
Spindle View
The spindle plays a pivotal role in the meiotic maturation of the human egg cell (oogenesis). It is responsible for the proper alignment and distribution of the chromosomes during cell division. In 15-20% of all cases, the mature eggs do not have a spindle prior to being fertilized by sperm. Besides the 1st polar body, the presence of a spindle is an accurate indicator of oocyte maturity. The older the women, the more frequently such spindle abnormalities are encountered. The absence of the spindle is associated with significantly reduced fertilization rates and poor or non-existent embryonic development. Spindle orientation during ICSI/IMSI has a decisive influence on further embryonic development. Usually the spindle is oriented in such a way that the 1st polar body is at the 12 o'clock position and the sperm cell is injected into the oocyte at the 3 o'clock position. If the spindle is not optimally positioned (in the majority of cases the spindle is close to the 1st polar body and thus located at a distance from the direction used for sperm injection) and is accidentally touched with the glass capillary during the microinjection procedure, this may lead to the destruction of the oocyte. In cases of repeated fertilization failure, great importance should be accorded to the spindle view (to be individually discussed and arranged with the attending physician).
Assisted Hatching
This method is aimed at facilitating the hatching of the developing embryo from the zona pellucida (outer shell of the embryo). The procedure involves making a small incision into the zona pellucida with the aid of a laser beam. This is particularly useful in cases where a pronounced thickening (detectable by so-called polarized light microscopy and standard light microscopy) of the zona is observed by the biologist or, where zona hardening is suspected. Especially with increasing female age, the egg coatings become thicker and harder. The same holds true for the zona of frozen-thawed embryos. Depending on the individual situation, the technique is used in our IVF laboratories only on a case-by-case basis.
PICSI
PICSI is a method of selecting mature sperm for use with ICSI/IMSI. The heads of mature sperm have a specific receptor that responds to hyaluronic acid (hyaluronan). Hyaluronan is naturally occurring as an essential component of the coating that surrounds the oocytes. Immature sperm do not have such a receptor. The so-called hyaluronic acid binding assay (PICSI) uses the fact that mature spermatozoa are able to bind to hyaluronan. Thus, mature spermatozoa can be separated from immature spermatozoa. These HA-bound sperm can be used for ICSI/IMSI. This technology is only used in very specific cases. PICSI cannot be a substitute for the IMSI technique, but in certain cases it can be regarded as an instrument to complement it.
Polarization Microscopy
The outer shell of the oocyte (zona pellucida) consists of 3 layers of glycoproteins surrounding the oocyte, or respectively, the embryo until it hatches from this shell. This happens on the 5th or 6th day of embryogenesis at the blastocyst stage of development. Using a polarization microscope, the zona can be evaluated with regard to the thickness of all three layers. These data allow for a better assessment of the properties of the zona of oocytes (or embryos). Especially the inner layer of the zona pellucida seems to be an important non-invasive marker for predicting oocyte development potential.
Initial medical consultation
Depending on the causes of the infertility in the woman/man, there are different therapy options available. During a personal medical consultation, it will be clarified which treatment is best suited to bring about the desired outcome.