Unerfüllter Kinderwunsch
Die menschliche Fortpflanzung
1. Der weibliche Zyklus
2. Fruchtbarkeit und weibliches Alter
3. Spermienproduktion
1. Der weibliche Zyklus
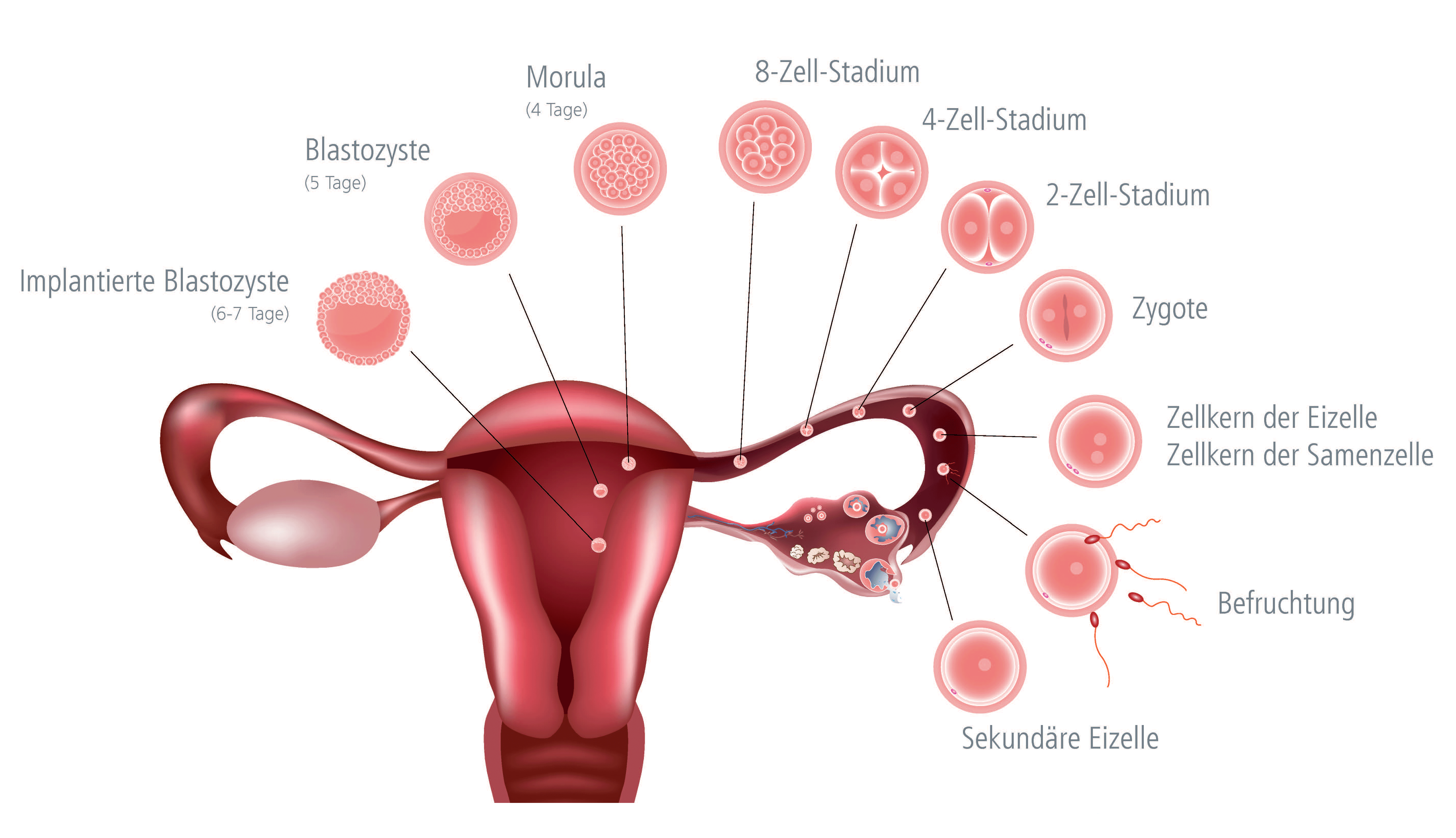
Ein Zyklus beginnt am ersten Tag der Monatsblutung. Jeden Monat reift in einem der beiden Eierstöcke eine Eizelle in einem Eibläschen (Follikel) heran. Schon im Vorzyklus beginnen sich mehrere Eibläschen (im Durchschnitt 10-12 Stk.) für den Eisprung im folgenden Monat zu entwickeln. Meist gelangt nur eines zur vollen Reife, während die anderen verkümmern.
Ausgereift ist das Eibläschen ca. 2 cm groß, gefüllt mit Follikelflüssigkeit. Die Eizelle befindet sich in der Wand dieses Follikels. Die maximale Größe wird in der Zyklusmitte erreicht. Um den 14. Tag öffnet sich der Follikel und entlässt die Eizelle gemeinsam mit der Follikelflüssigkeit in den Eileiter (Eisprung oder Ovulation). Mit Hilfe feinst gesteuerter Muskelkontraktionen und feinen Härchen (Zilien) an der Innenwand des Eileiters wird die Eizelle dann in Richtung Gebärmutter transportiert.
│ © 2021 Shutterstock/Next Fertility IVF Prof. Zech
Kommt es um den Zeitpunkt des Eisprungs zum Geschlechtsverkehr, so wandern die abgegebenen Samenzellen von der Scheide durch die Gebärmutter bis in die obersten Abschnitte der Eileiter. Nur ein einziges Spermium befruchtet die sich dort befindende Eizelle.
Die befruchtete Eizelle, welche nun Embryo genannt wird, beginnt sich bereits im Eileiter zu teilen und gelangt im Durchschnitt 5 Tage nach dem Eisprung in das Innere der Gebärmutter, wo sie damit beginnt, sich einzunisten.
Die Schleimhaut der Gebärmutter wird in jedem Monatszyklus neu auf das Einnisten des Embryos vorbereitet. Das sich entwickelnde Eibläschen produziert das Hormon "Östrogen". Je grösser das Bläßchen wird, desto höher steigt der Östrogenwert an. Dieses Hormon ist verantwortlich für das Wachstum der Schleimhaut der Gebärmutter bis zum Eisprung.
Nach dem Eisprung wandelt sich das Eibläschen in den sogenannten Gelbkörper um (dies geschieht durch die Granulosa-Zellen, welche die Bläschenhöhle auskleiden und nach dem Eisprung zum Gelbkörper werden). Der Gelbkörper bildet das Hormon "Progesteron", welches die Gebärmutterschleimhaut so umwandelt, dass sich der Embryo bei seiner Ankunft in der Gebärmutter gut einnisten kann.
Danach beginnt der Embryo den Signal-Stoff HCG abzusondern (HCG ist jenes Schwangerschaftshormon, welches im Urin oder im Blut gemessen werden kann und eine positive Schwangerschaft anzeigt = Schwangerschaftstest).
Der Embryo ist in den ersten 10-12 Tagen nach der Einnistung noch so klein, dass das HCG noch nicht messbar ist. Für den Gelbkörper aber sind die Signale stark genug, sodass er zu wachsen beginnt und immer mehr Progesteron bildet. Dieser Vorgang ist notwendig, da es sonst zu einer Blutung kommen würde.
Gelbkörperschwäche
Eine unzureichende Produktion von Progesteron ist ganz normal, wenn sich kein Embryo einnistet, denn in diesem Falle fehlen seine Signale. Der Gelbkörper beginnt zu schrumpfen und mit dem Abbluten der Schleimhaut kommt es zu einem neuen Zyklus. Das Einsetzen der Regelblutung kann wie das Start-Signal für einen neuen Zyklus gesehen werden. Dies alles wird durch einen sehr komplexen Regulations- mechanismus zwischen Eierstöcken, der Hirnanhangsdrüse (Hypophyse) und übergeordneten Zentren im Gehirn gesteuert.
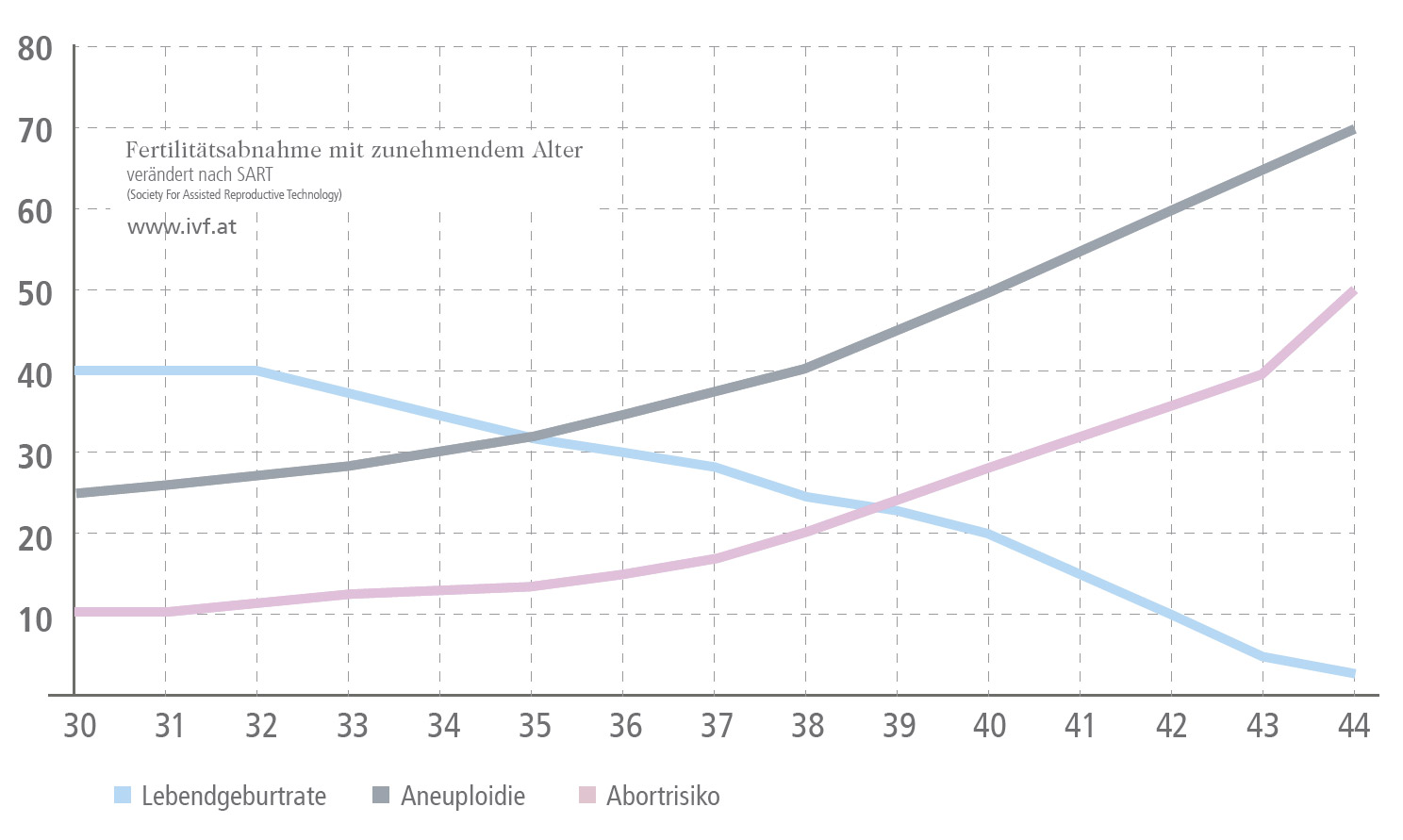
2. Fruchtbarkeit und weibliches Alter
Das Maximum der natürlichen Fruchtbarkeit der Frau wird im Alter von ca. 25 bis 35 Jahren erreicht. Nach dem 38. Lebensjahr sinkt die Fruchtbarkeit. Ab dem 43. Lebensjahr sind die Aussichten auf eine natürliche Schwangerschaft leider deutlich reduziert. Den größten Einfluss auf die weibliche Fruchtbarkeit haben Quantität und Qualität der Eizellen, die aber mit zunehmendem Lebensalter abnehmen.
Ein weiterer Punkt, der mit zunehmendem Lebensalter der Frau eine große Rolle spielt, ist ein erhöhtes Risiko für Veränderungen der Chromosomenzahl (Aneuploidie - zu viele, oder zu wenige Chromosomen) in der Eizelle. Nach der Befruchtung einer davon betroffenen Eizelle, ist die Embryonalentwicklung eingeschränkt und die Einnistung des Embryos in die Gebärmutter findet oftmals nicht statt. Kommt es dennoch zur Schwangerschaft, bleibt diese selten intakt, kann jedoch zur Geburt eines genetisch erkrankten Kindes führen.
Abnahme der Fertilität mit zunehmendem Alter
│ © 2021 Next Fertility IVF Prof. Zech
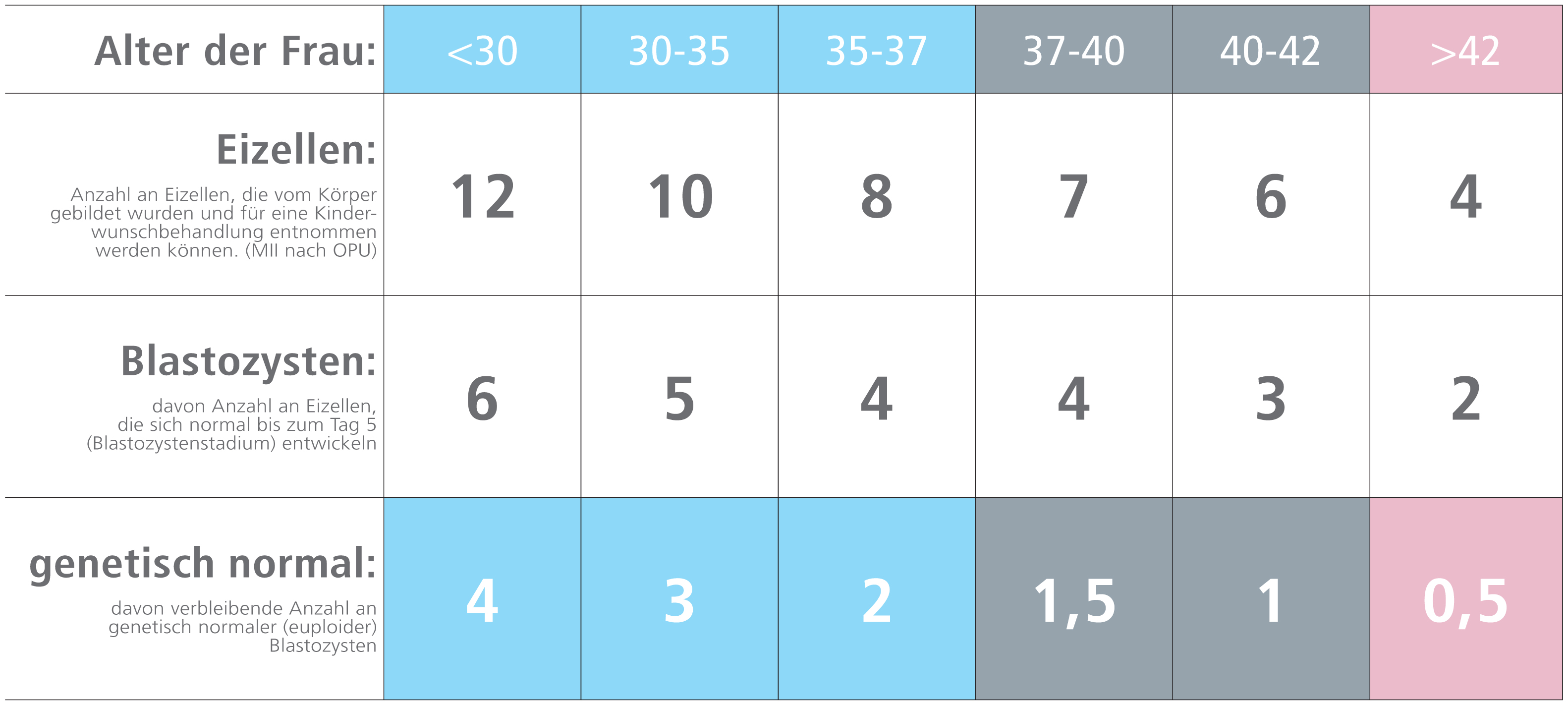
Anzahl an Eizellen und Entwicklungspotential nach Alter
│ © 2021 Next Fertility IVF Prof. Zech
3. Spermienproduktion
Bei einem gesunden, jungen Mann werden bis zu 100 Millionen Spermien pro Tag produziert. Die Entwicklung der Spermien findet in den Hoden statt und ist beeinflusst von zwei wichtigen Hormonen, nämlich dem LH und dem FSH. Diese Hormone werden von der Hirnanhangdrüse (Hypophyse) gesteuert. Das FSH bewirkt die Reifung in den Hodenkanälchen, das LH wird benötigt für die Entstehung des Testosterons im Gewebe und an den verschiedenen Stellen der Spermienproduktion. In den vergangenen Jahrzehnten war ein normales Spermiogramm mit mehr als 50 Millionen Spermien/ml angegeben. Die aktuellen WHO-Kriterien sprechen von einer heutigen Spermiendichte von 15 Millionen Spermien/ml. Dies zeigt, dass die Anzahl der Spermien in den vergangenen Jahren drastisch abgenommen hat. Im Hoden werden pro Sekunde etw. 1200 Spermien produziert. Die Entwicklung eines Samenfadens bis zum Verlassen aus dem Hoden beträgt ca. 3 Monate. Die Verbesserung der Samenqualität (oder auch des IMSI-Befundes) durch medikamentöse oder andere Maßnahmen ist nach Ablauf dieses Zeitraums zu erwarten.
Paare mit Kinderwunsch, die nach einem Jahr mit regelmäßigem Geschlechtsverkehr nicht schwanger werden, sollten eine medizinische Abklärung der Ursachen in Betracht ziehen.